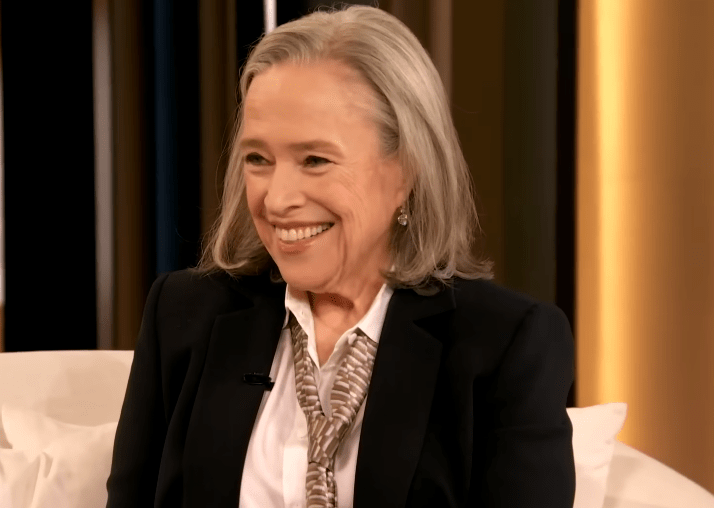
Credit: The Drew Barrymore Show
Kathy Bates’s weight-loss story is more akin to a meticulous, long-term public health case study than a celebrity makeover, as her family history, medical diagnosis, and everyday decisions come together to reimagine her energy and viability as an actor whose job requires perseverance; With a 2017 diagnosis of type 2 diabetes and the history of breast and ovarian cancer, she turned fear into strategy by gradually replacing burgers, pizza, and soda with well-balanced meals, paying attention to her body’s cues, and using walking as the most dependable form of exercise to maintain regular movement.
The clinical trigger is important because Bates saw relatives, including a father who lost a limb, suffer from diabetes, and this familial shadow made the diagnosis immediately actionable rather than abstract. Fearful, she adopted a patient, incremental approach that was especially helpful because it relied on long-term habits rather than drastic, short-term fixes. This approach helped her lose about 80 pounds through lifestyle changes before a GLP-1 medication helped her lose the remaining 15 to 20.
| Label | Information |
|---|---|
| Name | Kathy Bates |
| Born | June 28, 1948 — Memphis, Tennessee, USA |
| Occupation | Actress, director, producer |
| Career Highlights | Academy Award for Best Actress (1990); iconic roles including Misery; recent lead role in Matlock (CBS reboot) |
| Significant Health History | Ovarian cancer (2003); breast cancer with double mastectomy (2012); subsequent lymphedema |
| Key Turning Point | Type 2 diabetes diagnosis (2017) — prompted sustained lifestyle change and medical management |
| Methods Credited | Intuitive eating, stopping late-night meals, walking and low-impact exercise, patience, plus GLP-1 medication (Ozempic) to assist with final weight loss |
| Results | Approximately 100 lb lost over several years; reduced lymphedema symptoms; improved stamina for long shoots and stage work |
| Impact | Practical example of survivorship care, preventive action, and the nuanced use of medical aids alongside behavior change |
| Reference | https://people.com (People coverage and interviews cited) |
She stopped eating after 8 p.m., adopted intuitive eating habits from family—waiting five minutes after a meal to detect the stomach’s small sigh of satiety—and gave herself treats. Her method, which is straightforward and almost modest, is both humane and instructive. It kept compliance plausible over years rather than collapsing into cycles of deprivation and rebound, a practical approach that nutritionists frequently refer to as more durable for long-term maintenance.
Lymphedema, the post-cancer swelling that restricted Bates’s mobility and comfort for years, was functionally improved by the weight loss; less mass and inflammation around the affected limbs meant fewer days requiring compression sleeves, more clothing options that fit without difficulty, and an ease on set that she describes with delight, noting that walking between takes is no longer a punishing chore but a manageable task that makes long shoots feasible and creatively freeing.
Simple headlines are complicated by her candor regarding medication: Bates has been explicit that Ozempic, an FDA-approved GLP-1 agent for type 2 diabetes, helped with the last phase of weight loss, but she insists the heavy lifting was the years of diet and movement choices preceding it; framed this way, the drug appears as an adjunct—a clinical nudge rather than a magic bullet—a depiction that aligns with medical guidance stressing combined lifestyle and pharmacologic care for chronic metabolic conditions.
An emotional detail that defies sensationalism and instead suggests identity recalibration is the story’s human, almost cinematic moment: trying on dresses for the 2024 Emmy Awards with a friend and crying when clothes fit differently. The tears were a private acknowledgement that physical ease can restore dignity and confidence, which in turn affects opportunities and willingness to take on demanding roles.
During Harry’s Law, Bates had to sit in between takes to save energy. Now, she reports that she has the stamina to stand through scenes, move naturally in lengthy courtroom takes, and perform without the constant need for rest. Producers and directors respond to this kind of dependability, and by being notably more physically capable, she has expanded the range of characters she can play, an industry effect that is subtly persuasive for older actors navigating casting biases.
Walking as the main cardio, basic strength training to maintain muscle mass, and the realization that occasional indulgence is a part of a sustainable regimen are her refreshingly normal approaches to food and exercise. This combination works remarkably well because it addresses both physiology and psychology, avoiding the resentment that strict diets engender while producing consistent caloric deficits and metabolic improvements.
Bates’s measured commentary helps refocus the debate by highlighting the context: GLP-1 drugs, such as Ozempic, help people with metabolic disease and can be effective when combined with lifestyle changes, but they also require monitoring and carry the risk of weight regain if stopped. This nuance is often lost in social feeds where headlines simplify complex interventions into moral judgments. The public conversation surrounding these drugs has been noisy and moralizing.
Insightful parallels can be drawn from comparisons with other well-known survivors and athletes: success often follows a combinatory model—diagnosis, behavioral change, social support, and targeted medical therapy—which implies that integrated survivorship plans involving dietitians, physiotherapy for lymphedema, and access to evidence-based medical aids when necessary should be given priority in systems of care. Bates’s experience, when presented honestly and modestly, makes a strong case for that integrated model.
Additionally, her story reframes aging and fitness in a positive way, challenging narratives that reduce health investment to cosmetic motives. Bates frames her decisions as forward-thinking and pragmatic, stating that she wants to work more easily, avoid complications, and continue to be artistically active. This makes the arc motivational for fans and peers who may mistake weight loss among older adults for vanity rather than a strategy to preserve vocation and quality of life.
Because survivorship increasingly requires infrastructure rather than willpower alone, policymakers and insurers should pay attention to the social-policy angle that emerges from celebrity disclosures. When well-known individuals talk about survivorship care and routine monitoring, demand for certain services increases, exposing access gaps such as rehab services, physiotherapy for lymphedema, and affordable chronic-disease management.
The low-gloss authenticity of Bates’s story is also noteworthy; she identifies minor strategies, such as waiting for a post-meal sigh and going back to a routine after indulging, and she embraces imperfection. These anecdotes humanize the regimen and make it more approachable for readers who might otherwise reject celebrity makeovers as unattainable or excessive.
In the end, the storyline—diagnosis leading to change, years of consistent progress, cautious medication to complete the job, and return to demanding professional work—reads as a realistic, hopeful blueprint; it’s a model that persuades without reprimanding, that teaches a patient, evidence-based way to improve health and preserve craft, and that provides an upbeat, forward-looking message about how seasoned performers can maintain productive careers while managing chronic illness with dignity.

