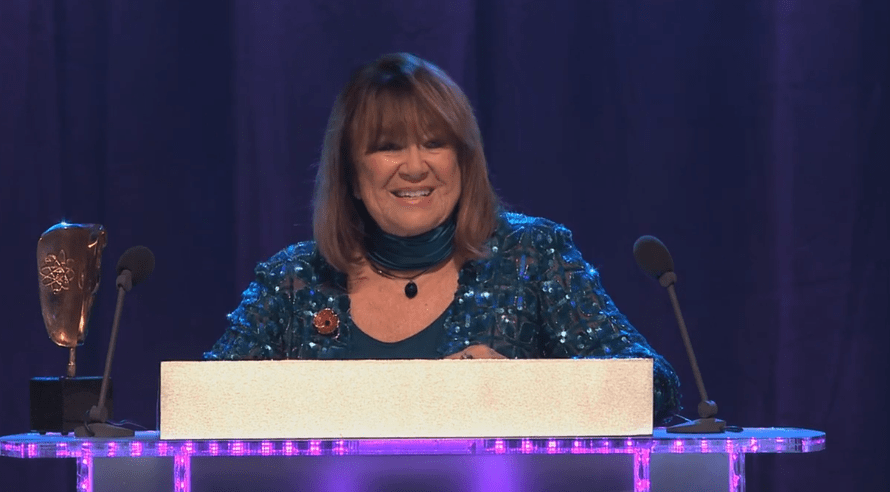
Credit: BAFTA
The cruciate ligament she felt snap that day was the first in a ten-year series of treatments, missed diagnoses, and ultimately, life-changing surgery. Her story serves as a warning and a guide for anyone who views pain as a minor annoyance rather than a call to action. Nerys Hughes’ injury, which was simple enough to describe but significant enough to change her perspective on work, aging, and healthcare, began as a routine crouch for a low camera on set.
The story is noteworthy not because the injury was uncommon but rather because the journey from audible snap to complete knee replacement is remarkably similar to too many patient narratives where early conservative treatment buys time but not resolution. She continued to work after that fall, a decision born of professional obligation and a stoicism ingrained by a career spent on tight schedules and the fragile rhythms of television production. However, that determination subtly amplified structural damage, setting in motion osteoarthritis that would later migrate to both knees and, eventually, neighboring joints.
| Label | Information |
|---|---|
| Name | Nerys Hughes |
| Born | 8 November 1941 — Rhyl, Flintshire, Wales |
| Occupation | Actress; narrator; stage and television veteran |
| Notable Credits | The Liver Birds (Sandra Hutchinson); The District Nurse (Megan Roberts); Doctor Who; Torchwood; The Queen’s Nose |
| Publicly Noted Health Issues | 2005 knee ligament injury from a fall on set leading to arthritis; bilateral knee replacements; type 2 diabetes (managed by tablets); concerns about osteoporosis; bunions; hiatus hernia |
| Recovery & Advocacy | Prepared carefully for staged full knee replacements with physiotherapy; regained mobility; patron of the National Osteoporosis Society; promotes prehab, rehab and realistic self-care |
| Personal Life | Married to cameraman Patrick Turley (since 1972); two children; splits time between homes in London and France |
| Reference | Wikipedia |
Hughes’ medical history sometimes resembles a ledger of treatments that alternated between symptomatic solutions and delayed structural repair: steroid injections, followed by gold, MRIs that revealed cartilage erosion that may have been exacerbated by years of kneeling in a garden without cushions, and finally the candid admission—repeated by a surgeon’s direct remark—that her knee “looked like jelly,” which prompted the decision to proceed with staged full replacements that would eventually restore function and alleviate pain.
Hughes discovered something clinically logical but culturally underappreciated while preparing for those surgeries: prehabilitation is important. Strengthening the thigh muscles before surgery and committing to the strenuous exercises following surgery are not optional niceties but rather the practical currency of recovery. The surgeon’s insistence that Hughes walk stairs shortly after an epidural-assisted procedure was both frightening and, looking back, the turning point that turned expectation into quantifiable improvement.
Hughes’ appreciation for a surgeon who combined skill with clear instruction reveals how much outcomes depend on that coordinated choreography rather than on solitary endurance. That rehabilitation sequence contains a quiet lesson: effective recovery is not a single heroic moment in theater but rather a swarm-like collaboration — surgeons, physiotherapists, nurses, family, and the patient moving together like a swarm of bees, each tiny action cumulatively rebuilding balance and mobility.
Her openness about secondary conditions lends helpful realism to the celebrity-health narrative. Hughes, who was diagnosed with type 2 diabetes ten years ago and is managing it with metformin and dietary changes, provides a relatable template for people juggling multiple health priorities by modeling a practical acceptance of chronic illness that avoids melodrama but insists on responsibility. She talks about avoiding crash diets, learning to count carbohydrates, and choosing walks and functional exercise over gym routines.
When an admired performer discloses osteoporosis, bunions, or the uncomfortable reality of a hiatus hernia, listeners are more likely to recognize symptoms earlier, seek second opinions, and demand imaging rather than accept injections as a long-term solution. This combination of lived detail and practical advice is the kind of public testimony that shifts social norms. The publicity value of a celebrity is useful in this situation precisely because it translates clinical detail into public curiosity, which in turn leads to earlier presentation and better results.
Hughes’ path into advocacy was natural rather than theatrical: she spoke warmly and with a certain modest fervor about her aunt who suffered from osteoporosis with dignity, and the charitable work she supports is based on the realities of peer support and community education rather than grandstanding. She also felt that becoming a patron of the National Osteoporosis Society was a moral and emotional next step after witnessing family members and acquaintances struggle.
Her story has ramifications that go beyond personal rehabilitation. Instead of being a moralizing grievance, Hughes’ story serves as evidence for a larger case for regular safety inspections, easily accessible imaging pathways, and the ability to pause filming without facing a career penalty. The production set where she was hurt, like many workplaces that depend on bodies and schedules, now appears to need clearer protocols, and her memory of continuing to work after a significant trauma invites managers and unions to reconsider duty-of-care practices.
The cultural arc is sharpened by comparisons with other public figures. When athletes or musicians take time off for health reasons, the public discourse frequently shifts from rumors to policies — from talking about a cancelled performance to questioning why support systems didn’t work. Hughes’ experience falls somewhere along that spectrum, illustrating how the entertainment industry needs to shift from requiring heroic endurance to establishing systems that enable prompt medical intervention and long-term careers.
Lessons pertaining to policy are particularly noteworthy. Hughes’ relatively quick transition from MRI to specialist surgeon may not be universal, so her call for early intervention and prehab has real policy force. Funding pre- and post-operative rehabilitation, cutting down on imaging wait times, and investing in community physiotherapy can all result in fewer long-term disabilities and lower societal costs. Access to timely orthopaedic assessment and joint replacement varies greatly across regions and healthcare models.
The case serves as an invitation for clinicians to speak honestly: stress the importance of strengthening muscles prior to surgery, be very clear about realistic recovery schedules, and challenge the cultural belief that “toughing it out” is a career-appropriate approach. Delays in definitive care can increase disability and costs, both financial and personal, and Hughes’ own admission that “I should have had the knee replacements much earlier” is a concise public health warning about missed windows.
Her testimony also has an emotional rhythm that is significant; she personalizes perseverance rather than dramatizing suffering, which is a heartwarmingly human combination. Anecdotal flourishes, such as Mollie Sugden’s story of using her handbag to beat an overly familiar fan during a public appearance or Hughes’ minor domestic regrets about gardening without protection, help readers envision realistic changes rather than impersonal directives.
In the end, Nerys Hughes’ illness and recuperation serve as a civic asset: a convincing argument for improved care pathways, a pragmatic supporter of prehab and rehab, and an illustration of how a public figure can transform personal suffering into the common good without resorting to theatricality. If her story is taken seriously, it encourages employers, clinicians, and policymakers to create systems that prioritize long-term involvement over temporary productivity gains. It also provides people with a realistic roadmap for transforming a diagnosis into restored mobility—not by chance, but through coordinated care, consistent effort, and the quiet bravery to make a change when it would have been easier to remain silent.

